Clinical Description and Manifestations
Andersen-Tawil syndrome, first described in 1971 in a case report by Andersen and later described by Tawil in 1994 is now universally recognized as a rare, multisystem disorder characterized by a triad of clinical features—periodic paralysis, dysmorphic features, and ventricular arrhythmias. ATS is a heterogenous disorder that is sporadically or autosomal dominant–derived and has a high degree of variable phenotypic expression and incomplete penetrance, with as much as 20% of mutation-positive carriers being nonpenetrant. The mean age of onset for periodic paralysis has been reported to be 5 years (range, 8 months to 15 years) and slightly older, 13 years (range, ~4 to 25 years) for cardiac symptoms.
Electrocardiographic abnormalities of ATS may include pronounced QTc prolongation, prominent U waves, and ventricular ectopy, including polymorphic ventricular tachycardia (VT), bigeminy, and bidirectional VT. Although ventricular ectopy is common and the ectopic density can be high in some patients, most ATS patients are asymptomatic and SCD is extremely rare. ATS1 was initially proposed as type 7 LQTS (LQT7) because of the observation of extreme prolongation of the QT interval; however, these measurements included the prominent U wave. As such, this complex clinical disorder, manifesting at times with only a modest prolongation of the QT interval, is probably best considered as its own clinical entity, referred to as ATS1 rather than as part of the LQTS regime. However, given the potential for false interpretation of the QT interval because of the prominent U wave and the probability of phenotypic expression of only cardiac-derived symptomatology (e.g., syncope, palpitations, ventricular rhythm disturbances), a considerable number of ATS patients are conceivably misdiagnosed with classic LQTS. Similarly, the presence of bidirectional VT, an accepted hallmark feature of CPVT (see later) often leads to a misdiagnosis of ATS as the potentially lethal disorder CPVT. Correctly distinguishing between ATS and CPVT is critical, because the treatment strategies are different.
Genetic Basis for Andersen-Tawil Syndrome
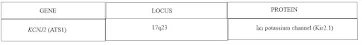
To date, over 30 unique mutations in KCNJ2 have been described as causative for ATS1. Mutations in KCNJ2 account for approximately two thirds of ATS, but the molecular basis of the residual third of ATS cases remains genetically and mechanistically elusive. Localized to chromosome 17q23, KCNJ2 encodes for Kir2.1, a small potassium channel alpha subunit expressed in brain, skeletal muscle, and heart, that is critically responsible for the inward rectifying cardiac IK1 current (see Table 9-1 and Fig. 9-1). In the heart, IK1 plays an important role in setting the heart's resting membrane potential, buffering extracellular potassium, and modulating the action potential waveform. Most KCNJ2 mutations described in ATS are missense mutations that cause a loss of function of IK1, either through a dominant negative effect on the Kir2.1 subunit assembly or through haploinsufficiency as a result of protein trafficking defects.
Table 9-1:
Fig 9-1:
Cardiac action potential disorders. Illustrated are the key ion currents (white circles) along the ventricular cardiocyte's action potential that are associated with potentially lethal cardiac arrhythmia disorders. Disorders resulting in gain of function mutations are shown in green rectangles and those with loss of function mutations are shown in blue rectangles. For example, whereas gain of function mutations in the SCN5A-encoding cardiac sodium channel responsible for INa lead to LQTS, loss of function SCN5A mutations result in BrS, CCD, and SSS.











No comments:
Post a Comment